Fellas – Listen Up! You Have A Pelvic Floor Too.
In my work treating women I sometimes see male partners who attend as a support person. I am always bemused that so many of these men are blissfully unaware that they too have pelvic floor muscles, and think they are only bestowed on women. I wonder how these men think they maintain continence but it is quite likely they have never had cause to think about that issue at all. After all, only 13% of Australian men will experience urinary incontinence as opposed to 37% of Australian women.1
Yes guys, listen up! This one’s for you … men can have pelvic floor problems too.
Let’s start with a quick check of the location and function of the pelvic floor muscles.
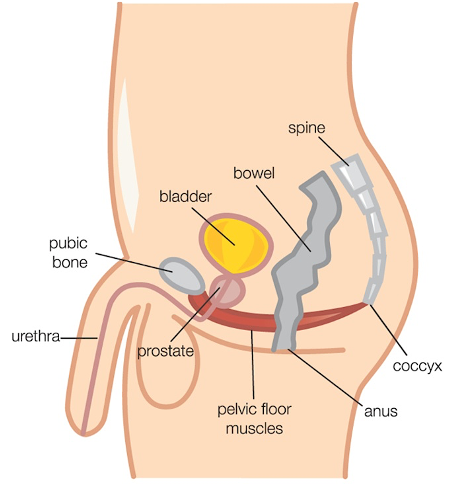
In both men and women, the pelvic floor muscles are a group of muscles sitting in the base (or floor) of the pelvis. They span from the pubic bone at the front of the pelvis to the tailbone at the back, and also extend side to side to just inside the “sit” bones. That’s a pretty big area. We all have layers of pelvic floor muscles – some that are deeper and some more superficial – with a network of connective tissue (fascia) interweaving through them.
The pelvic floor muscles have several important jobs in both sexes:
- Helping to maintain continence (prevent leakage) for the bladder and bowels
- Supporting the pelvic organs from below (in men that’s the bladder, bowel and prostate)
- Contributing to “core control” along with the other muscles
- Contributing to sexual function
However, we all know men and women are anatomically different, so of course there are some important differences between male and female pelvic floor muscles too.
The most obvious difference is the number and size of exit spaces through the pelvic floor. Everyone has openings for the urethra and rectum to pass through the pelvic floor to allow bladder and bowel emptying respectively. For men, with only one exit for the urethra and a narrower pelvis, the exit space in the front part of the pelvic floor is relatively small. Women, of course, have an extra opening for the vagina, and tend to have a wider pelvic inlet. These differences partly account for why women are more likely to have urinary incontinence and prolapse. Pregnancy and birth also make a difference too, as both cause considerable load on the pelvic floor muscles and fascial supports.
The role of the superficial pelvic floor muscles also differs significantly in men and women. In women, the superficial pelvic floor muscles contract during orgasm. However, for men, several of these superficial pelvic floor muscles are the ones that help maintain an erection, expel semen, and squeeze out the last drops of urine when emptying the bladder. So you can see why you need these muscles to work well.
We have already mentioned that men can have pelvic floor problems too. But are they the same kinds of problems seen in women and what do you need to watch out for?
Bladder Symptoms in Men
The most common urinary symptoms men will encounter relate to obstruction of urine outflow. This is most often caused by prostate enlargement or prostate cancer. An enlarged prostate can constrict the urethra as it passes through the prostate, preventing adequate bladder emptying. If this happens you might notice slowing of the urine stream, the need to strain to empty, dribbling after you think you’ve finished and increased urinary urgency and frequency. This needs immediate medical attention, as prostate cancer is the most common cancer in men and still kills around 3500 Australian men every year. We know prostate checks aren’t the most pleasant of experiences, but at least you’ll be alive to see the funny side of it later.
It is essential to get treatment for prostate cancer, which often involves either a prostatectomy (removal of the prostate) or radiotherapy. Unfortunately, these treatments can cause incontinence in some men. This occurs because surgery may damage or require the removal of parts of the urethral sphincter muscles along with the prostate, and both surgery and radiotherapy can sometimes damage the nerves and other supporting tissues in the pelvis too. Official reported rates of post-prostatectomy incontinence are up to 70%. With radiotherapy, just under 40% of men may experience urinary leakage.2
Bowel Symptoms in Men
Even though urinary leakage is more common in women than men, it is a different story when it comes to bowel symptoms. About 20% of Australian men will suffer faecal incontinence, compared with just under 13% of Australian women.1 Up to 27% of men and women suffer constipation. Bowel leakage and constipation can be linked, partly because all that straining can end up stretching and damaging the pelvic floor muscles, including anal sphincter muscles and supporting fascia. However, a poor diet lacking in fibre, lack of exercise, bowel disease (eg, IBS, Crohn’s disease) and surgery on the bowel, including surgery for bowel cancers can also contribute to bowel troubles.
Sexual Symptoms in Men
Erectile dysfunction (ED) is the most common, although not the only, sexual dysfunction for men. It is more common than many men like to think, with 40% of men experiencing ED over their lifespan.3 Many people don’t know that ED is commonly linked to heart disease and disorders such as diabetes, so it is really important to see your GP if you experience this problem. ED is also very common after prostatectomy. Removal of the prostate will mean men no longer have ejaculate fluid, but it is the inability to get an erection that can be most troubling. ED usually takes longer to improve than post-prostatectomy incontinence but can be treated.
Pelvic Pain in Men
Chronic pelvic pain (CPP) in women is becoming increasingly better recognised, especially disorders like endometriosis. CPP encompasses pain in the pelvis that has been there for at least 3-6 months. Men can also suffer from CPP, but many have never even heard of it. This can make it hard to know who to turn to for help. Studies suggest up to 18% of Australian men may suffer from CPP,4 although true figures may be higher, as it is often poorly diagnosed and under-reported. In men, CPP is often called “prostatitis” but it is not always related to inflammation of the prostate gland as that name suggests.
Symptoms of CPP in men can mimic some other pelvic health disorders, including difficulty emptying the bladder and bowels, and frequent toilet trips in an attempt to urinate. But men with CPP can also experience a range of other symptoms including pain in the testes, penis, anus, abdomen or groin, pain with sitting, and pain with intercourse or orgasm. Guys, if you have CPP you should always see your GP as the first point of call, as some of these symptoms can be related to infections or other problems. But if nothing is found, be sure to ask for information on CPP.
How can a physiotherapist help?
A pelvic health physiotherapist can assist men with all types of pelvic health problems.
To manage urinary or bowel incontinence following prostate cancer, bowel surgery or from other causes, the major focus of treatment will usually be learning to strengthen and use the pelvic floor muscles for functional support. How you need to do these exercises will differ slightly depending on whether the problem is related to bladder or bowel control. For bladder control try to “shorten the penis” or “stop the flow” when doing exercises (but don’t practise actually stopping the flow more than once a week). For bowel control aim to “stop wind” and lift under the testes. Many surgeons now recommend seeing a physiotherapist before surgery to learn how to contract the pelvic floor muscles effectively, to aid better post-op recovery. A pelvic health physio will also look at things like good bladder and bowel habits and how to empty the bowels without straining.
For erectile dysfunction, a pelvic health physio can also recommend pelvic floor exercises and general exercise to improve erectile support and blood flow to the region. Men who don’t respond well to medications like Viagra may also benefit from devices like penile pumps to help restore erectile function
Just as in women, treating CPP in men is best managed by a multi-disciplinary team. Pain education is vitally important, along with relaxation strategies, general exercise and stress management. Learning how to relax the pelvic floor muscles is often helpful for many men with CPP.
I hope this has helped you to understand that not only do blokes have pelvic floor muscles, but they can suffer from pelvic floor problems too. The good news is they can be treated. The first step is asking for help – that’s often the hardest part.
Please pass this information on to the important men in your life. You never know, it might just help them take that difficult first step.
Yours in pelvic health.
Jenny.
References:
- Continence Foundation of Australia
- NICE guidelines: Lower urinary tract symptoms in men overview 2020.
- RACGP
- Pitts et al (2008) Prevalence and correlates of three types of pelvic pain in a nationally representative sample of Australian men. J Sex Med
